“I am type B. I can’t donate blood for your surgery. We need to find another donor.”
Have you ever wondered what it is that determines your blood type or why it’s so important for doctors to know their patient’s blood type before transfusion? Let’s learn as much information as we can. The International Society of Blood Transfusion (ISBT) recognizes, until this point, 36 human blood group systems. This means that every individual can classify their blood into 36 different categories, based on antigens that are found on the surface of their red blood cells (erythrocytes). However, when we talk about our blood group, we usually refer to two blood group systems, only. These are the ABO system and the Rhesus system. Let’s find out more.
Antigens
Antigens are molecules that can be found on the surface of our cells. When you hear the word antigen, you might think of it as something bad, often connected to pathogens such as a virus that causes an immune reaction to protect our body. Antigens, though, are not always bad. Our own cells can have markers on their surface that participate in physiological functions. These markers are considered antigens, otherwise known as self-antigens since the immune system does not recognize them as foreign. Such antigens can be proteins, carbohydrates, glycoproteins, or glycolipids. When scientists studied the 36 blood group systems, they found that 346 different antigens exist in the human population. What makes us individuals different from each other though? Why can two different people have different antigens on their red blood cells and consequently belong to different blood groups? The answer lies in our genes; the antigens are inherited. Therefore, the genes we inherit from our parents, code for the specific antigens that are present on our cells.
The ABO system
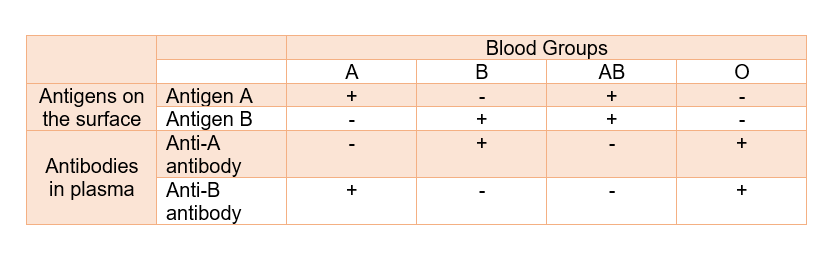
According to the ABO system, there are four possible blood groups. These are A, B, AB, and O. The antigens that are responsible for this classification are called antigen A and antigen B. As their names suggest, people carrying the antigen A on their red blood cells have type A blood, those that have the antigen B, have type B blood, while those that have both A and B antigens belong to the AB type of blood. Instead, type O people have neither the A antigen nor the B. What’s interesting is that the type of antigens that is present on the erythrocytes determines the kind of antibodies that the immune system produces against other blood types. The plasma of a person having type A blood contains antibodies against the antigen B, which we call anti-B antibodies. This means that the body produces antibodies against the antigens that are absent from its erythrocytes. Therefore, people with type B blood, have anti-A antibodies. Furthermore, type AB people, whose blood contains both A and B antigens, have no antibodies at all. On the other hand, people that belong to the O type of blood have anti-A and anti-B antibodies because the respective antigens are absent from their cells. You can find this information in a more comprehensible way on the following table:
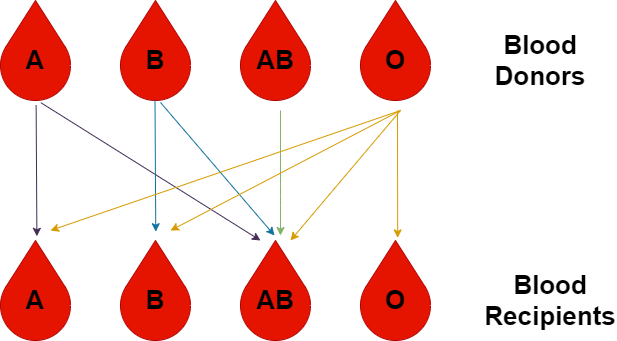
As you may have already guessed, the kind of antibodies that is present in our blood is the reason why not all blood types can always be used for transfusion into a particular patient. If we mix a certain type of blood, let’s say type A containing A antigens, with serum containing anti-A antibodies in the lab, we will observe a process called agglutination. The anti-A antibodies recognize the A antigens, against which they are produced in the first place and they destroy them. The same will happen inside the body if we transfuse type A blood in patients with type B blood, whose plasma contains anti-A antibodies. When these antibodies meet the foreign antigens, agglutination will occur because the immune system will attack the donor red blood cells, posing a threat to the patient’s health. For the above reasons, we need to make sure the donor’s and the recipient’s blood are compatible before any transfusion. This means that only certain types of blood can be given to people according to their blood type as we can see in the picture below:
Genetics of the ABO system
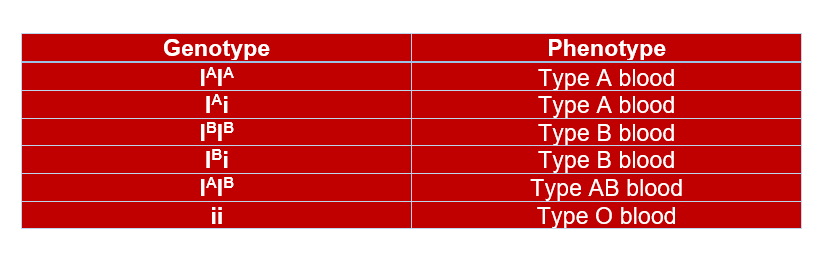
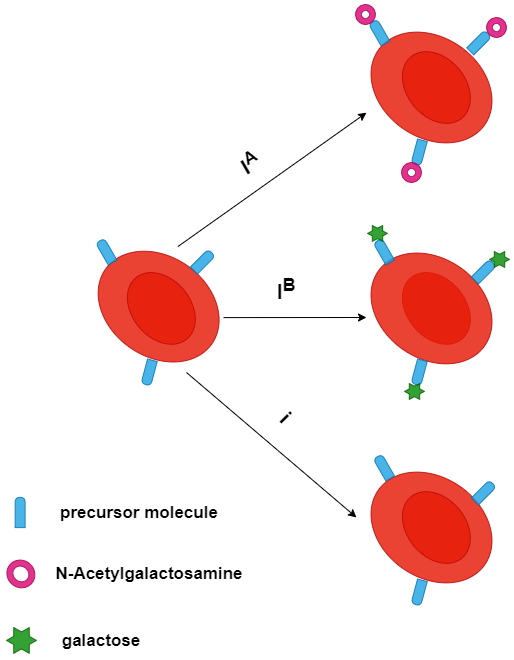
There is one genetic locus located on chromosome 9 responsible for the determination of one’s blood group according to the ABO system. This locus contains multiple alleles, specifically, three alleles: IA, IB, and i, coding for a glycosyltransferase, an enzyme modifying a precursor molecule on the surface of red blood cells. The i allele is the recessive allele while the IA and IB are dominant over i. Additionally, IA and IB are codominant. This means that the genotype IAIB results in a phenotype where both alleles are expressed. But, how do the enzymes encoded by these alleles give rise to the antigens that are present on our erythrocytes? The IA allele codes for an enzyme that transfers an N-acetylgalactosamine on the aforementioned precursor molecule, creating the A antigen. On the other hand, the IB allele codes for an enzyme that transfers a galactose on that molecule, forming the B antigen. The i allele codes for an inactive enzyme, meaning that the precursor molecule is not modified. According to the information we get about the ways the three alleles behave in different combinations, we can find the phenotype that results from each possible genotype. Each one of us has two alleles, one from our father and one from our mother.
The Rh system
In addition to the ABO system, it is also important to know how your blood is classified according to the Rhesus (Rh) system. There is a big number of antigens associated with this system. But the most important one is the Rh(D). The Rh(D) antigen or factor can be either present or absent on the surface of the red blood cells and the indication used to describe what is the case for each individual is ‘positive’ and ‘negative’, respectively. The Rhesus status can be presented along with the ABO symbols that are accompanied by a + (positive) or – (negative) sign. For example, A+ means the A antigen and the Rh(D) antigen are present on the erythrocytes, whereas B- means the antigen B is present but the Rh(D) factor is absent. The presence or absence of the Rh(D) antigen plays a role in the compatibility of blood groups, so again we need to take this into consideration before any blood transfusion. Rh-negative blood can be donated to someone that has either Rh-negative or Rh-positive blood. However, Rh-positive blood can be donated only to people who have Rh-positive blood.
Complete table of compatibility
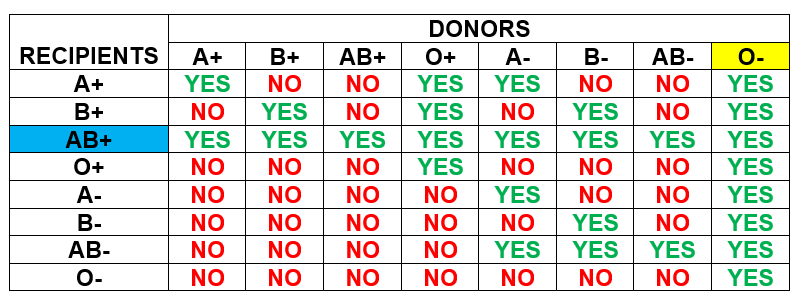
Studying the table above, we realize that AB+ is the universal recipient, which means people with this type of blood can receive blood from any group. On the other hand, O- is the universal donor, which means these people can donate their blood to any other blood group.