Bacteria often have bad fame since they are mostly known for the diseases they cause to the human population. However, not all bacteria are bad. A large number of bacteria live inside our bodies or on the surface of our skin, without us being aware of them. This is because they are necessary for our well-being, comprising the normal flora. In this chapter, though, we will only discuss the pathogenic bacteria that can sometimes put our lives in danger. Our immune system is responsible for fighting off infections caused by bad bacteria, as does with all the other pathogens that can end up in our bodies. Scientists, though, have been able to find a way to assist the immune system in its effort to kill these bacteria with the use of pharmaceutical substances, called antibiotics.
What are antibiotics?
Antibiotics are medications used for the prevention and treatment of bacterial infections. The word antibiotic comes from the Greek anti and biotic (or bios), which essentially means against life. That name causes a common misconception that antibiotics can be used against any pathogenic microorganisms or viruses. In reality, though, they are simply antibacterial substances, which means they can only be used against bacteria. When someone is infected by viruses, fungi, or protozoa, they must not be prescribed antibiotics or take over the counter antibiotics without their doctor’s permission. For the last decades, though, this has not always been the case. There is a large number of people that take antibiotics without needing them. The antibiotic medication will not treat their infection unless it is a bacterial one. In addition to that, it will contribute to a very serious problem, called antibiotic resistance. This is an issue that has been a case for the last couple of years, and it will only get worse unless we stop the imprudent and excessive use of antibiotics, since bacteria can acquire resistance against them and we will not be able to kill them.
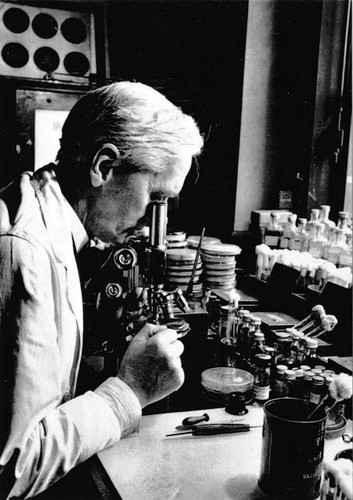
Antibiotics can be divided into many categories based on different features. They can be classified as natural antibiotics, which are produced by microorganisms found in nature or as synthetic antibiotics that are made in the lab. One of the most popular antibiotics and the first one to be discovered is penicillin. Penicillin was discovered by Alexander Fleming in 1928. Fleming was studying staphylococcal bacteria when one day, he noticed that inside a Petri dish that had been contaminated with mold spores, the bacteria had died. On the contrary, the bacteria that were farther away from the mold had survived. He realized that the mold had some kind of antibacterial activity. This particular mold was a fungus, belonging to the Penicillium genus, and had the ability to produce penicillin. Penicillin saved many lives as it was used for treating infections of soldiers during World War II. Now, it is the most widely used antibiotic, and it has treated many serious infections such as pneumonia, gonorrhea, syphilis, and meningitis.
Antibiotics can also be divided to wide-spectrum antibiotics that can be prescribed against a wide range of bacteria, and narrow-spectrum antibiotics that target only specific types of bacteria. Another useful classification of antibiotics is associated with their mechanism of function. Different antibiotics target different molecules and cellular functions. Therefore, they can be either bacteriostatic, which means they stop the bacterium from growing, or bactericidal, which means they result in the death of the bacterium.
Basic structure of bacterial cells
In order to understand how an antibiotic can kill bacteria or just inhibit their growth, we need to take a look at the basic structure of bacterial cells. Except for a small number of bacteria that do not have a cell wall, most of the others are divided into two categories based on their cell wall structure. These are Gram-positive and Gram-negative bacteria. These names are derived from the way the bacterial cells behave during a staining procedure carried out in the lab, which we will not concern ourselves with. As every cell, both Gram-positive and Gram-negative bacteria are surrounded by a plasma membrane. In the case of Gram-positive bacteria, outside of the plasma membrane, there is a thick cell wall composed of peptidoglycan. On the other hand, outside of the plasma membrane of Gram-negative bacteria, there is a thin layer of peptidoglycan. The peptidoglycan layer is in its turn, surrounded by another lipid bilayer, called outer membrane, which contains lipopolysaccharides as well.
The plasma membrane helps in the maintenance of the bacterial components inside the cell and regulates the intracellular conditions by preventing ions from flowing freely in or out of the cell. The cell wall gives the cell its shape and protects it from pressures in both Gram-positive and Gram-negative bacteria. However, the outer membrane that is present in Gram-negative bacteria contains channels that can let various substances, including drugs, inside the cell. In the cytoplasm of both Gram-positive and Gram-negative bacteria, many cellular processes take place, including three very important functions: DNA replication, transcription of DNA to RNA, and translation of mRNA into proteins.
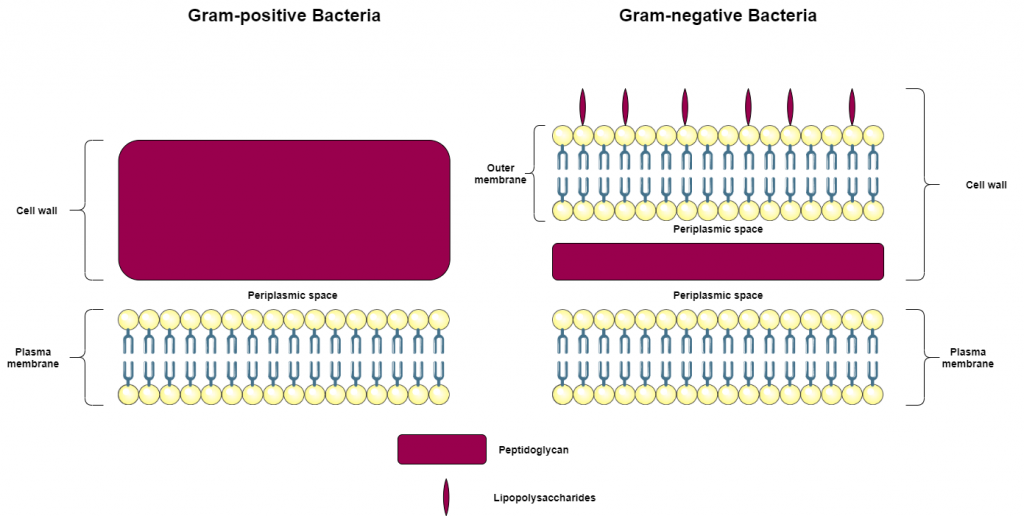
On the right: Cell wall structure of Gram-negative bacteria
(Lipid bilayer by Servier Medical Art under a Creative Commons Attribution 3.0 Unported License)
How antibiotics work?
We mentioned before that antibiotics can be either bacteriostatic or bactericidal. What is the factor that determines what happens when an antibiotic attacks a bacterium? It depends on the antibiotic’s molecular target. In a few words, if the bacterium is able to survive without the function that is being inhibited by the antibiotic, then the antibiotic is called bacteriostatic, and it just prevents the bacterium from growing, making it easier for the immune system to destroy it. Alternatively, if the bacterium is not able to survive because a very important function is compromised by the antibiotic, then the antibiotic is considered bactericidal and results in the death of the bacterium.
According to their mode of action, antibiotics can be divided to:
- Cell wall synthesis inhibitors
- Cell membrane disruptors
- DNA and RNA synthesis inhibitors
- Protein synthesis inhibitors
- Folic acid metabolism inhibitors
1. Cell wall synthesis inhibitors
The cell wall is, in both types of bacteria, made of peptidoglycan. In order, though, for the peptidoglycan strands to be composed, a series of reactions must occur. β-lactams and glycopeptides are two classes of antibiotics that can inhibit this process. Penicillins and cephalosporins are widely used β-lactams. These have the ability to bind to PBPs, proteins that take part in a step of peptidoglycan synthesis, and therefore inhibit the synthesis. A well-known glycopeptide is vancomycin, which binds to the substrate of PBPs, and inhibits the process as well. In both cases, the cell wall cannot be synthesized, and the bacterium dies.
2. Cell membrane disruptors
The cell membrane can also be vulnerable when exposed to antibiotics. Polymyxin B is a bactericidal antibiotic used against Gram-negative bacteria, since it can disrupt phospholipids of the outer membrane first and the inner membrane afterward, resulting in cellular components leaking outside of the cell. Another example of antibiotics targeting the plasma membrane is daptomycin, which is used against Gram-positive bacteria. Daptomycin disrupts the membrane potential by causing depolarization. This means that K+ (potassium ions) are released to the extracellular environment and kill the bacterium because the selective permeability of the membrane is lost. Therefore, the osmotic balance is disrupted.
3. DNA and RNA synthesis inhibitors
a) DNA synthesis inhibitors
Fluoroquinolones are bactericidal antibiotics that inhibit DNA replication. During DNA replication, an enzyme called gyrase or topoisomerase is necessary for the creation of the replication fork. Fluoroquinolones such as ciprofloxacin inhibit this enzyme, preventing the DNA from being replicated.
b) RNA synthesis inhibitors
Antibiotics can also be used for the prevention of RNA synthesis. RNA is synthesized during a process called transcription with the use of DNA as a template. The enzyme that transcribes DNA is called RNA polymerase. Rifamycin is an antibiotic that has the ability to bind to the RNA polymerase and block the initiation of transcription so that no mRNA can be produced.
4. Protein synthesis inhibitors
Protein synthesis takes place in the bacterial ribosome, a ribonucleoprotein complex consisting of two subunits, the 30s and the 50s subunit.
Tetracyclines and aminoglycosides such as streptomycin are two groups of antibiotics targeting the 30s subunit, and more specifically, a site called A site. Aminoglycosides cause the misreading of mRNA, and consequently, the premature termination of translation, while tetracyclines prevent the tRNA molecules from binding to the ribosome, therefore, inhibiting translation. Aminoglycosides are bactericidal and tetracyclines are bacteriostatic antibiotics.
Chloramphenicol is an antibiotic that binds to the 50s ribosomal subunit and prevents the peptide bond formation so that the protein cannot be produced. Macrolides are another class of antibiotics that bind to the 50s subunit. Erythromycin belongs to this class and causes a premature release of incomplete peptides.
5. Folic acid metabolism inhibitors
Folic acid is a very important molecule for the production of nucleotides, and therefore, the synthesis of DNA. Sulfamethoxazole is an antibiotic belonging to the class of sulfonamides. It binds to an enzyme called dihydropteroate synthase, inhibiting the formation of a precursor molecule that normally leads to folic acid. Trimethoprim is an antibiotic that inhibits dihydrofolate reductase, the enzyme that forms tetrahydrofolic acid (the active form of folic acid) from dihydrofolic acid. Trimethoprim is a bacteriostatic antibiotic when used on its own. However, when used in combination with sulfamethoxazole, it is believed to kill the bacteria.
Sources: