In a previous post, we talked about antibiotics and how they have helped us fight off bacterial infections since their discovery in 1928. To this day, they are used for the prevention and treatment of mild to severe infections some of whom were once dangerous or even deadly. Even though they are life-saving substances, they are the reason behind a very serious problem that will concern us for many years. This problem is called antibiotic resistance and is a major threat to public health. The term antibiotic resistance does not mean that our body resists against the function of the prescribed antibiotics, as many people mistakenly believe. It means that the bacteria that we are trying to target with antibiotics during an infection become resistant against the antibiotics and manage to ignore their presence, thus survive and continue to grow inside the infected individual. In other words, it seems that antibiotics are no longer as effective as they used to be for the fight against bacteria. Furthermore, the misuse and overuse of antibiotics will only make things worse.

What is antibiotic resistance?
Antibiotic resistance is not a new phenomenon. It has been a case since ancient times and is the result of evolution. More specifically, it is the result of a basic law of Darwin’s theory, the survival of the fittest. What does that mean exactly, and how does it occur? Antibiotics, except for synthetic ones that have recently been made in the lab, are produced by organisms found in nature. As a consequence, even before humans started using antibiotics in medicine, bacteria used to be exposed to them by other organisms around them. If the bacterial cells were susceptible to the antibiotic action, they would die. We know one of the fundamental characteristics of all living organisms is the struggle for survival. Therefore, bacteria, which possessed functions that enabled them to avoid the antibiotic action, would be able to survive, multiply, and become numerous in the overall bacterial population. This is the same thing that happens in our time when we use antibiotics to treat bacterial infections. Bacteria are exposed to those substances, and some of them may acquire characteristics, which make them resistant to specific antibiotics.
Mechanisms of antibiotic resistance
We know that antibiotics can bind to certain molecular targets and disrupt essential cellular processes. But how can a bacterium become resistant to one or more antibiotics? How can it overcome the antibiotic’s action? How is it possible that a previously considered bacteriostatic or bactericidal antibiotic does not affect the bacterium anymore? Bacteria can follow four strategies, each one including subcategories that contribute to the antibiotic resistance:
- One often-used mechanism is the prevention of the antibiotic entrance in the bacterial cell. The antibiotic’s target molecule may reside in the cytoplasm, the periplasmic space, or the inner membrane depending on the type of bacterium and the type of drug. In order to reach their targets, antibiotics use porins, which are channels located on the cell membrane. So, bacteria can alter the type, levels of expression, or function of these porins to prevent the antibiotic from entering the cell. This way, the drug cannot find its target, and the bacterium survives. The same result can also be achieved even if the antibiotic manages to enter the cell. In this case, bacteria can use efflux pumps, which are machines that extrude the drugs to the external environment.
- Another strategy is the modification or destruction of the antibiotic. Antibiotics are chemical substances with a specific structure that allows them to recognize their targets. That’s why bacteria have developed enzymes that add specific chemical groups to the antibiotic compound. The modified antibiotic is now inactive as it no longer recognizes its target. An alternative solution is the use of enzymes that destroy the antibiotic instead of just modifying it.
- Antibiotic resistance is also developed when bacteria protect or modify the antibiotic’s target. The molecule that is recognized by the antibiotic may become altered due to mutations that occur in the gene by which it is produced. Another strategy is the use of enzymes that alter the site of the molecule to which the antibiotic binds. For example, enzymes can add specific chemical groups there. It’s also possible for the cell to replace the target with another molecule so that the cell is not affected by the antibiotic.
- One very interesting method bacteria use to avoid antibiotics is to alter whole processes and mechanisms that take place inside the cell. That means they can follow alternative routes or chemical reactions to achieve the same functions as before without being in danger of the drugs. For example, if an antibiotic targets a molecule that is involved in the process of cellular energy, then the cell can adopt a new way of processing energy. That shows there is a global adaptive response inside the cell, not just the alteration of one molecule, as was the case with the three previous strategies.

How do bacteria gain those mechanisms of antibiotic resistance?
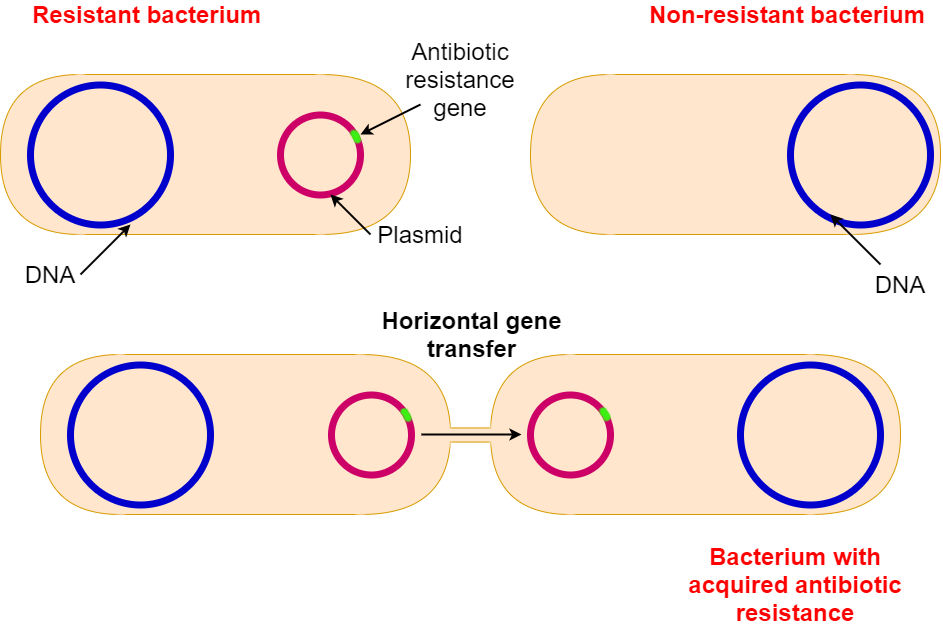
Bacteria can acquire the above mechanisms of antibiotic resistance through two possible ways, mutations and horizontal gene transfer (HGT).
A mutation is a random change in the DNA. Imagine you are reading a text on your computer and simultaneously copy it in your notebook. It is quite possible that as you write down the words, you can make one or more spelling errors or typos that will change the meaning of your text. The same thing can happen in bacterial DNA when it is replicated. This way, the information the DNA contains for, let’s say, the production of an enzyme is altered. That altered enzyme may now have the ability to bind to an antibiotic and destroy it, protecting the cell from its action.
Horizontal Gene Transfer is a function presented by bacteria during which small DNA molecules such as plasmids, are transferred between bacterial cells. The DNA molecules that are exchanged may possess genes that contribute to antibiotic resistance. For example, bacterium A has a plasmid containing an antibiotic resistance gene. If bacterium A meets bacterium B, HGT may occur and the plasmid is transferred to bacterium B, making it resistant to that particular antibiotic as well.
No matter the way a bacterium gains antibiotic resistance, it will have an advantage compared to the non-resistant ones. The main reason why bacteria evolve so quickly in comparison to other organisms, including humans, is that bacteria have a short life cycle. Let’s look at this example. Approximately 30 years pass from the moment a human being is born until they have children of their own. However, in the case of bacteria, the generation time ranges from a few minutes to a few hours. As a consequence, we can see the effects of bacterial evolution almost immediately, since, for example, a bacterium that divides every 30 minutes equals to 48 generations in only 24 hours. An interesting fact is that Alexander Fleming was the first one to warn us about antibiotic resistance since not long after he discovered penicillin, he noticed that some of the bacteria he was studying started presenting resistance to the antibiotic.
Why should we be concerned by antibiotic resistance and what can we do about it?
It seems that antibiotic resistance makes bacterial infections harder to treat. Diseases we believed we had left behind, start to kill once again. The problem is even greater when the bacterial strains are multidrug resistant. That means they avoid the action of many commonly used antibiotics, not just one, leaving us with no alternative until new antibiotics are found, or another solution is developed. Immunosuppressed patients, like those that are being treated for cancer or those that have undergone transplantation, are in danger of becoming critically ill and die if they contract antibiotic resistant bacteria. Moreover, antibiotics are very important for the prevention of bacterial infections during surgeries. However, the presence of resistant bacteria makes this task difficult and puts many people in danger. Chronically ill people are at high risk, but otherwise healthy people are not always safe from this situation either. Therefore, we realize that antibiotic resistance is a great threat, and we have to be cautious. It is the responsibility of all of us to listen to specialists in the field and follow some guidelines so that we won’t contribute even more to the current problem. Some of them are:
- We must not take antibiotics when infected with viruses or other pathogens because antibiotics work only against bacteria.
- We must not demand antibiotics from our doctors to get better sooner because we will not get better unless the infection is bacterial.
- We must not take antibiotics that had been previously prescribed to other members of our family without consulting our doctor first, since not all antibiotics are right for all types of bacteria.
- We must not interrupt our antibiotic treatment before we take all of the prescribed doses, even if we start feeling better. This is because some of the bacteria may still be present in our body, and they may become resistant if we stop the medication.
Finally, don’t forget that there is a huge number of antibiotics that are good for our health inside our bodies, but they may also carry antibiotic resistance genes due to their exposure to antibiotics. Those genes might be transferred to pathogenic bacteria when we are infected and make those resistant as well. So keep in mind that when using antibiotics without following the right directions, you are making your own bacteria resistant and putting yourself and others in danger.
You can also visit:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4888801/ for more information on mechanisms of antibiotic resistance
https://www.fda.gov/consumers/consumer-updates/combating-antibiotic-resistance for an update from the FDA