Hemolytic Disease of the Newborn (HDN) is a type of anemia that occurs when the mother’s immune system attacks and destroys the fetal red blood cells as a result of an incompatibility between the mother’s and the baby’s blood group. Another term used for this condition is Erythroblastosis fetalis, but we will discuss the reason behind this name later in this article. We already know that the human blood can be categorized in a number of groups using different systems. You can find more information on this subject here. The human body produces antibodies against the antigens that are absent from its erythrocytes. Thus, this is an issue that concerns us during transfusions, but it is also important to take into consideration in the case of some pregnancies.
Rhesus incompatibility
When a woman is pregnant, her blood might be incompatible with her baby’s in several different blood group systems. Some of them are less important than others. However, the most dangerous case of incompatibility has to do with the Rhesus system. According to the Rhesus classification, our blood can be divided into different groups based on the presence or absence of antigens such as the D, C, c E, and e. However, the most serious condition happens when the mother and embryo differ regarding the D antigen.
People whose blood cells present the RhD antigen are classified as Rhesus positive (Rh+) whereas people in whom the antigen is absent are classified as Rhesus negative (Rh-). The allele coding for the RhD antigen is dominant, which means that people with a DD or Dd genotype are Rh+ while those that have a dd genotype are Rh-. Hemolytic disease of the newborn is possible to occur if the mother is Rhesus negative and is impregnated by a man that is Rhesus positive. Let’s take a look at the Punnett squares below to help us understand what are the probabilities of a Rh+ child to be conceived by a Rh- woman and a Rh+ man.
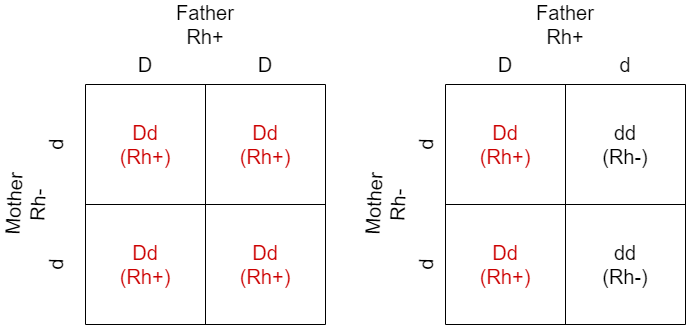
If the father is homozygous for the dominant allele (DD), there is a 100% chance the offspring will be Rhesus positive. If the father is heterozygous (Dd), there is a 50% chance it will be Rhesus positive. When the woman is Rh+, there is no problem regardless of the father’s genotype. Therefore, it is important to know the parents’ blood groups, as the mother might produce antibodies against the D antigen and attack her baby’s red blood cells.
First pregnancy
Let’s find out what happens when a Rh- mother gets pregnant for the first time with a Rh+ fetus. The mother and the fetus’s bodies are connected through the placenta that among others, participates in transferring nutrients to the developing embryo. What’s important to understand is that the placenta is structured in a way that does not allow the mother’s and the baby’s circulations to mix. A few fetal red blood cells can move across the placenta and end up in the mother’s circulation throughout the pregnancy. However, during delivery, the number of red blood cells that pass into the mother’s circulation elevates due to fetomaternal hemorrhage. These cells carry the Rh(D) antigen on their surface and are recognized as foreign by the mother’s immune system. Therefore, the mother is sensitized and an immune reaction takes place during which her immune cells produce anti-Rh(D) antibodies.
Since this is the first time her immune system encounters this particular antigen, the immune reaction is characterized as primary and the immune cells produce a small concentration of the antibody. It’s also useful to be aware that the antibodies that are produced in a primary response belong to a class of antibodies called IgM. A special characteristic of the IgM class is that it cannot pass through the placenta and pose a threat to the fetus. This way, the fetal red blood cells that are found in the mother’s circulation are destroyed without any harm coming to the fetus. However, memory B cells are produced in the mother’s body, the same thing that happens against other invaders such as pathogenic bacteria or viruses. The role of memory B cells is to act fast and produce a higher concentration of antibodies in case the body is exposed to the same antigen again in the future.
Childbirth is not the only cause of a Rh- woman’s immunization. Some other ways can lead to her sensitization against the RhD factor as well. For example, pregnancy with a Rh+ fetus that results in a miscarriage or an abortion, an ectopic pregnancy, or a significant fetomaternal hemorrhage as a result of trauma. It is also possible to occur when medical procedures such as amniocentesis or chorionic villus sampling are carried out. Furthermore, a woman can become sensitized without a pregnancy in case she is previously transfused with Rhesus positive blood for a different medical reason. This way, the transfused cells that carry the D antigen on their surface are recognized by her immune system.
Second pregnancy
If a woman that’s been previously, in one way or another, sensitized against the RhD factor gets pregnant again with a Rhesus positive fetus, it is possible that her immune system will attack the embryo’s erythrocytes. During the first weeks of the pregnancy, there is no threat for the embryo as its red blood cells do not express the D antigen on their surface yet.
Later on, though, fetal red blood cells can cross the placenta barrier and enter the mother’s circulation triggering her immune system. This time, a secondary response takes place, which means that her memory B cells produce anti-D antibodies of a different class, called IgG. IgG antibodies have the ability to be transported through the placenta and end up in the fetal circulation. This is a very important function of the placenta as it helps the embryo to acquire some of its mother’s antibodies to be able to fight off infections until it develops its own immune system after birth. Although this is useful in the case of antibodies against pathogens, the transport of anti-D antibodies to the fetus can cause serious disease, hemolytic disease of the newborn, as they will recognize the red blood cells and destroy them causing anemia. The hemolysis and the subsequent symptoms can vary from mild to severe and even the death of the fetus or newborn may occur.
When the baby is born, the signs of hemolysis are visible, usually in the first 24 hours, since the destruction of red blood cells causes jaundice, as a result of the bilirubin, a breakdown product of hemoglobin that ends up in the liver. Due to the massive destruction of the red blood cells, the newborn’s body tries to compensate by releasing immature red blood cells, called erythroblasts from the bone marrow. This is the reason behind the alternative name of HDN, erythroblastosis fetalis. Other organs such as the spleen and the liver try to produce red blood cells as well resulting in splenomegaly and hepatomegaly (enlargement of the spleen and liver, respectively). The disease can be so severe in some cases that it affects the function of vital organs such as the brain and the heart and can lead to the death of the newborn.
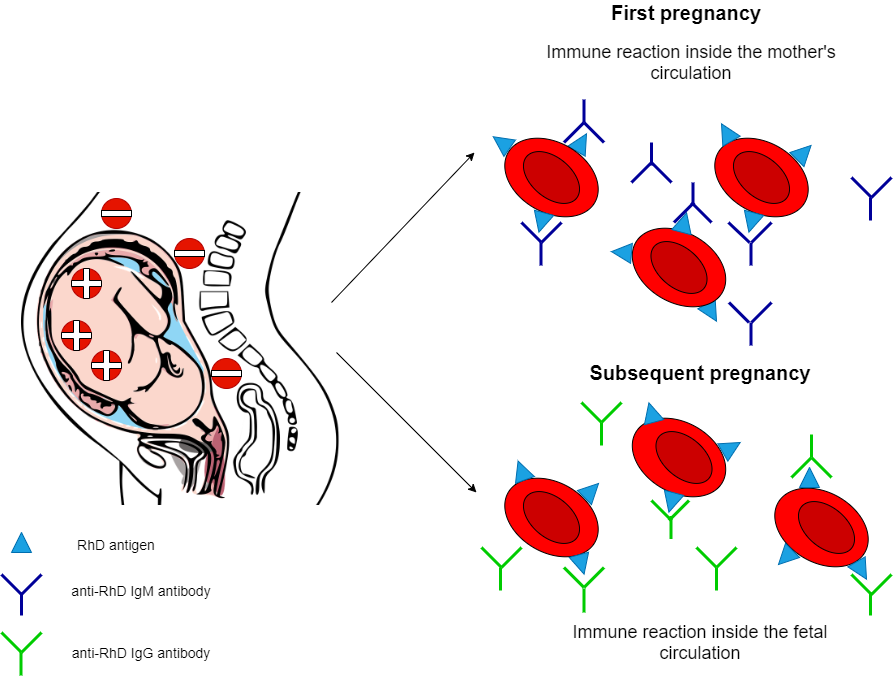
On the right: Immune reactions that occur when anti-RhD antibodies are produced against RhD antigens.
Diagnosis, Prevention, and Treatment
Hemolytic disease of the newborn is nowadays rare in the developed world thanks to the advancement of diagnostic techniques as well as treatments that help us prevent its occurrence or minimize its consequences. When a woman is pregnant, she is immediately tested to determine her blood type. If she is Rh-negative, the embryo’s father is also tested. If he is Rhesus negative as well, no further testing is needed, since the carrying fetus will also be Rh-. If however, the father possesses the RhD antigen, there is either a 50% or 100% chance the fetus will be Rh+ whether he is heterozygous or homozygous respectively. In these cases, the fetus is closely monitored throughout the course of the pregnancy.
Scientists have now developed an immunoglobulin, called RhoGAM, or Rh immunoglobulin that targets the RhD antigen without crossing the placenta and thus is used as a preventative measure. If the Rh- woman has not been sensitized previously and is pregnant with a Rh+ fetus, a specific dose of Rh immunoglobulin is administered to her so that it can destroy the fetal red blood cells that end up in her circulation without triggering an immune response. Consequently, no anti-D IgG antibodies can harm the fetus of a subsequent pregnancy. RhoGAM is used first at around the 28th week of the pregnancy when the D antigen starts to express on the cells’ surface. It is administered again 72 hours after delivery to ensure that any fetal blood cells that might be present in the mother’s body after childbirth are destroyed. RhoGAM is also used after a miscarriage, medical procedures, or other incidences that increase the likelihood of immunization.
It is important to note that if the woman is already sensitized, RhoGAM will not work and the only solution is to treat the baby’s condition. If while monitoring the fetus, doctors realize anemia is threatening the baby’s life, a blood exchange transfusion can be carried out inside the uterus so that the fetal blood that contains the anti-D antibodies is replaced with new blood. Moreover, if the baby is born with symptoms of HDN such as jaundice, phototherapy can be done to reduce bilirubin levels.
For more information on the subject, visit: https://www.ncbi.nlm.nih.gov/books/NBK2266/